This post may contain affiliate links to products or services which, if you purchase, may result in my earning commissions at no additional cost to you.
Written by Dr. Beau B Hightower
MS, DC, CSCS, CES
Migraine headaches are a cultural phenomenon that exceeds the normal reaches of media and cultural influence and seeps into the medical arena. If you ask an average person that is experiencing a “severe” headache they will tell you that they are having migraine headaches. Even family doctors and interns have a difficult time explaining what exactly differentiates a migraine headache from other types of headaches. Today we are going to discuss a common, yet poorly recognized type of headache that is beginning to make more and more noise in the media and in medical circles. This type of headache is called the “cervicogenic headache” which literally means that it originates in the cervical spine or neck.
The nerve that provides sensation to the skin and scalp of the human head is called the trigeminal nerve and transmits information to the brain via a nucleus in the spinal cord called the trigeminal nucleus. An anatomical “trick” in the body, the nerves from the upper 3 vertebrae in the neck share the same nucleus, which in layman’s terms means that our brains have a difficult time differentiating where pain is coming from in these regions. Much in the same way that heart attacks refer pain along the left arm, dysfunction and pain in the upper neck often refers pain into the skull and forehead. Contributing to the medical confusion is the fact that both cervicogenic and true migraines typically affect only one side of the head at a time
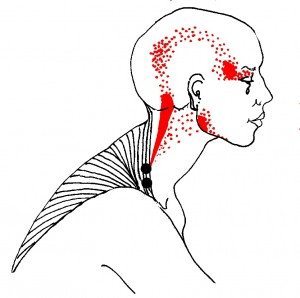
Patients that experience neck pain on the same side as their headache will often experience tightness from the upper cervical neck muscles which can reproduce the sensation of unilateral headache. This over activity in upper cervical spine muscles will often lead to restricted range of motion in rotation, which makes it difficult to turn the head to one side or sometimes both. Headaches of cervicogenic nature typically cause pain at the base of the skull and pain on the temple or around the eye.
These headaches are often misdiagnosed as migraines which means that your doctors may prescribe medications for the wrong type of headache. True migraines are often associated with numerous autoimmune neurological conditions or hormonal changes. These headaches are now thought to be of neurogenic origin, meaning they come from inside the brain. The brain itself does not contain pain fibers and this is why patients can be kept conscious during brain surgery operations. Commonly, it was thought that the blood vessels in the brain caused pain due to expansion and retraction, but new research is showing that this may not be the case.
An important finding concerning cervicogenic headaches, is that they can be reproduced by a clinician pressing manually on the upper cervical spine, especially the transverse process of C1 and C2. If you press on your lateral upper neck, and can feel pain similar to your headache, the headaches is more than likely coming from your neck itself.
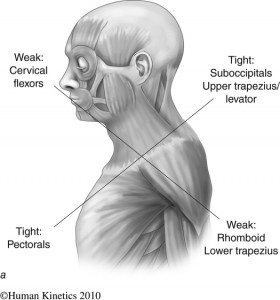
Upper crossed syndrome, is a condition in which our lifestyles cause an imbalance in the musculature in the shoulders and neck. The patient becomes weak in the rhomboids and lower trapezius muscles (the muscles between the shoulder blades) and feel as if they have a difficult time sitting up straight. As a result, the levator scapulae muscle is forced to hold the head upright and becomes thicker and fibrous and causes sharp pain at the superior and medial portion of the shoulder blade. This muscle attaches from the shoulder blade to the lateral upper three bones of the neck causing pressure at both attachments. The upper attachment point is the location that refers pain into the head and is the primary cause of cervicogenic headaches. Fascial connections exist between the suboccipital muscles and upper cervical dura, which attaches to the cranial fossa and C2 vertebra.
The most common ways to begin to correct these types of headaches is to consult with your local musculoskeletal expert who is familiar with Janda’s Movement Dysfunctions and to ask them which specific exercises can be done to correct this chronic presentation. Strengthening of the middle back muscles, and stretching/inhibition of the overactive muscles in the neck and chest will make dramatic changes, and self myofascial release using devices such as the myofascial stick on the lateral upper cervical musculature can relieve and even cure these types of headaches.
Finally, we need to discuss “Red Flag” presentations of headaches that would require immediate visits to a medical physician.
Red flag symptoms requiring further medical evaluation include:
~Headaches that are getting worse over time
~Sudden onset of severe headache
~Headaches associated with high fever, stiff neck, or rash
~Onset of headache after head injury
~Problems with vision or profound dizziness
For the millions of headache sufferers out there, there is hope in the fact that you may not actually have migraine headaches and there is a simple solution to cure your headache. Sometimes pain in the head can also be a big pain in the neck (literally).
Disclaimer: This article is for educational purposes only. If you have a medical condition, it is prudent that you seek medical evaluation by a properly qualified and licensed practitioner.
Dr. Beau Hightower is a former collegiate athlete and avid fight fan. He serves as the President of Elite Ortho-Therapy and Sports Medicine LLC, the premier sports injury resolution center in New Mexico. He serves on the Board of Directors for Parker University and their Alumni Association.
Elite-OSM.com